Bawasir in 2025: Myths, Facts, and the Future of Treatment


Updated on: 4th Jun 2024
Bawasir, commonly known as hemorrhoids or piles, continues to be a prevalent medical condition worldwide. Despite its prevalence, the condition is shrouded in myths, misconceptions, and stigma. With advancing medical research and treatment options, 2025 promises a brighter future for those suffering from Bawasir. This blog will debunk myths, provide factual insights, and explore the future of Bawasir treatment.
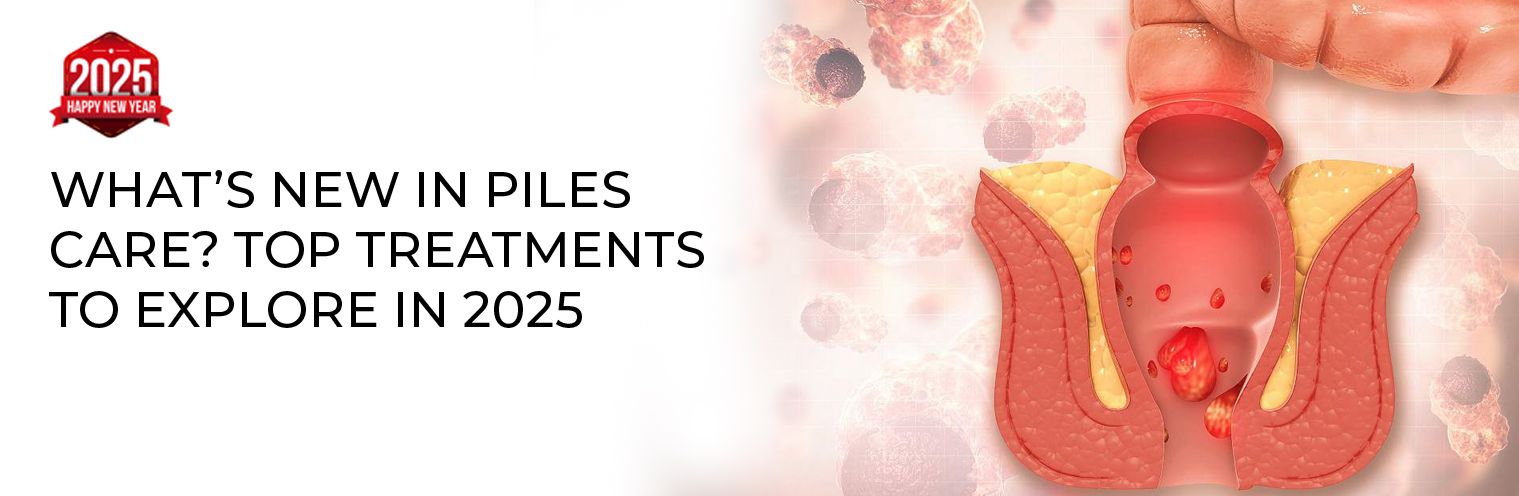
Understanding Bawasir
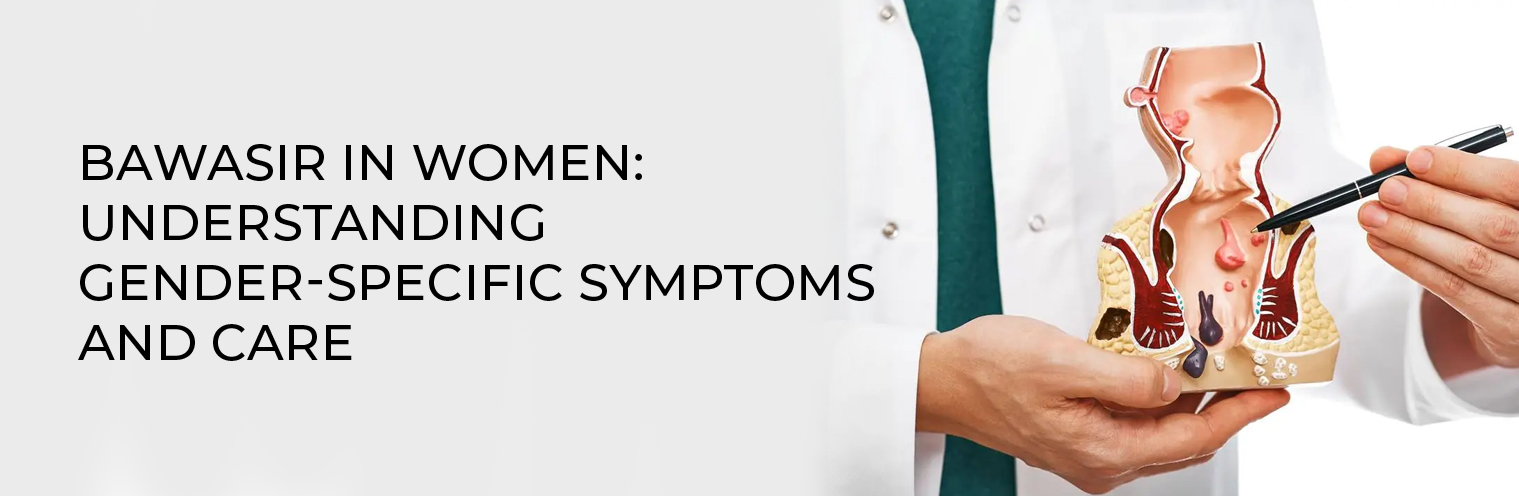
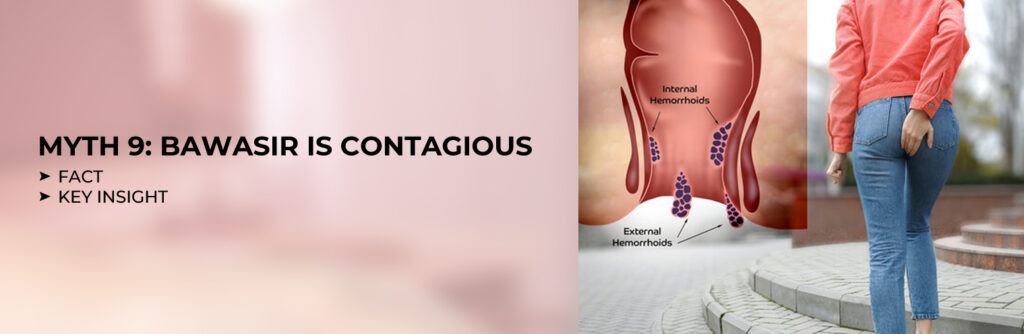
Bawasir refers to swollen veins in the rectum and anus that cause discomfort, pain, and sometimes bleeding. It is typically classified into two types:
- Internal Hemorrhoids: Located inside the rectum and usually painless but may cause bleeding.
- External Hemorrhoids: Found under the skin around the anus, causing pain, swelling, and itching.
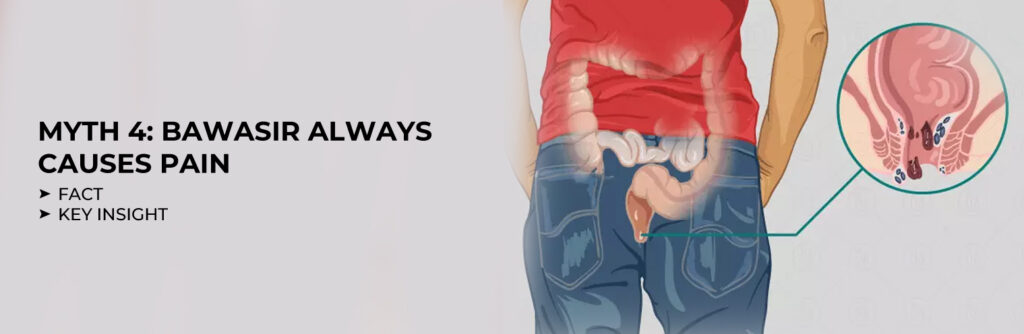
Common Myths About Bawasir

Myth 1: Only Older People Get Bawasir
Fact: While Bawasir is more common in individuals over 45, it can affect people of all ages. Factors like chronic constipation, pregnancy, obesity, and a sedentary lifestyle contribute to its development.
Myth 2: Spicy Food Causes Bawasir
Fact: There is no direct evidence linking spicy food to Bawasir. However, excessive consumption of spicy food can irritate the digestive tract, potentially worsening symptoms in those already affected.
Myth 3: Surgery is the Only Treatment
Fact: Surgery is one of many treatment options for Bawasir. Mild cases can often be managed with lifestyle changes, dietary adjustments, and non-invasive treatments.
Myth 2: Spicy Food Causes Bawasir
Fact: While mild cases may improve with time and care, chronic Bawasir requires medical attention to prevent complications.
Facts About Bawasir

Fact 1: A Common Condition
Bawasir affects approximately 4.4% of the global population, with many cases going unreported due to stigma and embarrassment.
Fact 2: Not Always Painful
Internal Bawasir often goes unnoticed because it is usually painless. External Bawasir, however, can cause significant discomfort.
Fact 3: Diet Plays a Crucial Role
A diet rich in fiber, fruits, and vegetables helps prevent constipation, a leading cause of Bawasir. Staying hydrated is equally important.
Fact 4: Advancements in Treatment
Recent years have seen significant advancements in Bawasir treatment, including minimally invasive procedures like rubber band ligation, laser therapy, and stapler surgery.
The Future of Bawasir Treatment in 2025

1. Personalized Treatment Plans
The advent of precision medicine is set to revolutionize Bawasir treatment. Tailored treatment plans based on a patient’s genetic makeup, lifestyle, and medical history will improve outcomes and reduce recovery time.
2. Minimally Invasive Techniques
- Laser Therapy: This painless, quick procedure effectively treats both internal and external Bawasir with minimal downtime.
- Stapler Surgery: A modern approach to treating prolapsed internal hemorrhoids, ensuring less pain and faster recovery.
3. Non-Surgical Alternatives
- Infrared Coagulation (IRC): A promising technique for early-stage internal Bawasir.
- Sclerotherapy: Involves injecting a solution into hemorrhoids, causing them to shrink.
4. Technology-Driven Solutions
- AI in Diagnosis: Artificial intelligence is aiding in the early detection of Bawasir, ensuring timely intervention.
- Telemedicine: Virtual consultations are making it easier for patients to seek advice without the embarrassment of face-to-face visits.
5. Integration of Ayurvedic and Holistic Treatments
Ayurveda continues to play a role in Bawasir management. Treatments like Kshar Sutra and herbal remedies are gaining acceptance for their effectiveness and minimal side effects.
6. Focus on Prevention
Awareness campaigns in 2025 will emphasize prevention. Simple lifestyle changes such as regular exercise, a high-fiber diet, and proper hydration can significantly reduce the risk of developing Bawasir.
How to Manage Bawasir Effectively

1. Dietary Adjustments
- Increase fiber intake through whole grains, fruits, and vegetables.
- Drink at least 8 glasses of water daily.
- Avoid excessive consumption of processed and fast foods.
2. Regular Exercise
Physical activity helps maintain healthy bowel movements and reduces the risk of constipation.
3. Good Bathroom Habits
- Avoid straining during bowel movements.
- Do not delay the urge to use the toilet.
- Limit the time spent sitting on the toilet.
4. Over-the-Counter Remedies
- Use creams, ointments, or suppositories designed for Bawasir relief.
- Sitz baths can alleviate pain and swelling.
5. Seek Medical Help When Needed
If symptoms persist or worsen, consult a healthcare professional to explore advanced treatment options.
Conclusion
Bawasir, though common and often misunderstood, is manageable with the right knowledge and care. As we move into 2025, advancements in medical science, technology, and holistic practices promise a future where Bawasir can be effectively treated and even prevented. By debunking myths, embracing facts, and staying informed about the latest treatments, individuals can take proactive steps towards better health and well-being.
Meet Our Specialists

Dr. Raj Kumar Garg (B.A.M.S.)
40+ Years of Experience

Dr. Rahul Garg (B.A.M.S.)
15+ Years of Experience