Piles Uncovered: Everything You Need to Know About Bawasir

Updated on: 4th Jun 2024
Piles, also known as hemorrhoids or bawasir, is a common medical condition affecting millions of people worldwide. Despite being a prevalent issue, it remains a taboo topic for many, leading to a lack of awareness and delayed treatment. In this comprehensive guide, we will uncover everything you need to know about piles, including its causes, symptoms, types, treatment options, and preventive measures.
What Are Piles (Bawasir)?
Piles are swollen veins in the lower rectum and anus, similar to varicose veins. They can develop inside the rectum (internal piles) or under the skin around the anus (external piles). The condition can cause discomfort, pain, itching, and sometimes bleeding, making daily activities challenging for those affected.
Causes of Piles

Several factors contribute to the development of piles, including:
- Chronic Constipation: Straining during bowel movements puts pressure on the rectal veins, leading to swelling.
- Prolonged Sitting: Sitting for extended periods, especially on hard surfaces, increases pressure on the anal region.
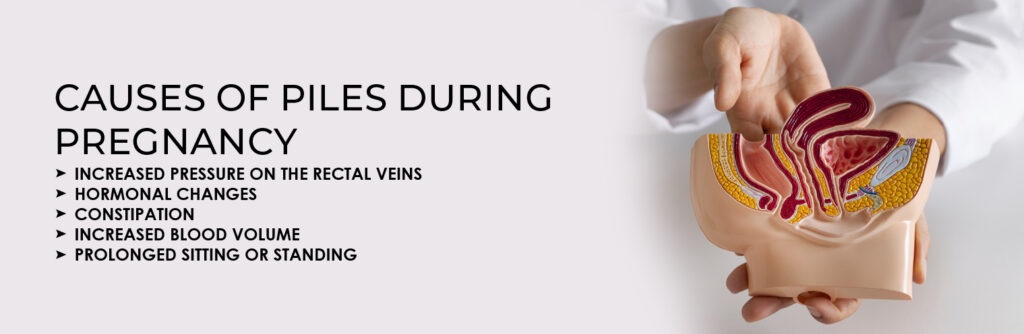
- Pregnancy: The growing uterus puts pressure on pelvic veins, increasing the risk of piles.
- Obesity: Excess weight puts additional strain on rectal veins.
- Low-Fiber Diet: A lack of fiber leads to hard stools, making bowel movements difficult.
- Heavy Lifting: Regularly lifting heavy objects can strain the rectal muscles.
- Genetic Factors: A family history of piles can increase the likelihood of developing the condition.
- Aging: As we age, the tissues supporting rectal veins weaken, making piles more common.
Symptoms of Piles

The symptoms of piles vary depending on their severity and type:
- Internal Piles: Usually painless but may cause bleeding during bowel movements.
- External Piles: Cause pain, itching, and swelling around the anus.
- Thrombosed Piles: Form when a blood clot develops in an external pile, leading to severe pain and inflammation.
- Prolapsed Piles: Occur when internal piles protrude outside the anus, causing pain and irritation.
Diagnosis of Piles
A doctor can diagnose piles through:
- Physical Examination: Inspecting the anal region for external piles.
- Digital Rectal Examination (DRE): Checking for internal piles by inserting a gloved finger into the rectum.
- Proctoscopy or Sigmoidoscopy: Using a small tube with a camera to examine the rectum for internal piles.
Treatment Options for Piles

Treatment depends on the severity of the condition and includes:
Home Remedies and Lifestyle Changes
- High-Fiber Diet: Eating fruits, vegetables, and whole grains helps soften stools.
- Hydration: Drinking plenty of water prevents constipation.
- Regular Exercise: Improves digestion and reduces pressure on rectal veins.
- Sitz Baths: Soaking in warm water can reduce pain and swelling.
- Avoiding Straining: Prevents additional pressure on the anal region.
Medical Treatments
- Medications: Over-the-counter creams, ointments, and pain relievers provide relief.
- Rubber Band Ligation: A small rubber band is placed around the base of the pile to cut off blood supply, causing it to shrink.
- Sclerotherapy: Injection of a chemical solution to shrink piles.
- Infrared Coagulation: Uses infrared light to shrink piles.
- Hemorrhoidectomy: Surgical removal of large or severe piles.
- Stapler Surgery: A minimally invasive procedure for treating prolapsed piles.
Prevention of Piles
Preventing piles involves adopting healthy habits such as:
- Eating a Fiber-Rich Diet: Ensures smooth bowel movements.
- Staying Hydrated: Keeps stools soft.
- Avoiding Prolonged Sitting: Taking breaks and moving around reduces pressure.
- Exercising Regularly: Promotes bowel health.
- Maintaining a Healthy Weight: Reduces strain on the rectal veins.
- Practicing Good Toilet Habits: Avoid straining and use soft toilet paper.
When to See a Doctor
Consult a doctor if you experience:
- Persistent bleeding during bowel movements.
- Severe pain or discomfort.
- A lump around the anus that does not go away.
- Symptoms that do not improve with home treatment.
Conclusion
Piles or bawasir is a common yet manageable condition. By understanding its causes, symptoms, and treatment options, individuals can take proactive steps to manage and prevent piles effectively. If symptoms persist or worsen, seeking medical advice is essential for proper diagnosis and treatment. With the right approach, relief from piles is achievable, ensuring a healthier and more comfortable life.
Meet Our Specialists

Dr. Raj Kumar Garg (B.A.M.S.)
40+ Years of Experience

Dr. Rahul Garg (B.A.M.S.)
15+ Years of Experience